![[Local data] A local review on childhood lead poisoning](/sites/default/files/styles/header_image_article_mobile/public/2019-11/image10_2.jpg.webp?itok=IzZfZ2EA)
Article
[Local data] A local review on childhood lead poisoning
Public health
3 min read
Background:
- Childhood lead poisoning is a key public health concern among different countries
- In 2015, a major health crisis happened in Hong Kong, where a number of public housing estates were found to have lead present in the drinking water
Possible sources of childhood lead exposure and poisoning:
- Natural source including air, dust, soil and water
- Industrial source including smelters, refineries, mines, lead gasoline, etc.
- Household water from copper plumbing with lead solder
- Human breast milk
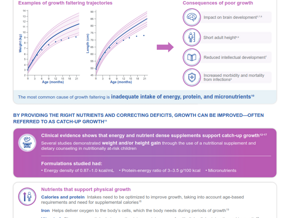
Clinical manifestations or complications of lead poisoning:
- Lead poisoning in the majority of children is asymptomatic
- Neurological manifestations: acute encephalopathy, hearing loss, neurobehavioral disorder such as hyperactivity, developmental delay, etc.
- Physiological complications: colicky abdominal pain, constipation, growth retardation, anemia, etc.
Screening for lead poisoning in children:
- The American Academy of Neurology: Children with developmental delay, including those with known identifiable risk factors for excessive lead exposure are suggested to be screened for lead toxicity
- Hong Kong government: Children aged under 12 years with a borderline raised blood lead level (5 mcg/dL*) should be conducted with lead exposure risk assessment and developmental assessment, while all citizens should be continuously monitored with raised blood lead levels
*correlates with the targeted screening promoted by the Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP)
Medical management strategies for childhood lead poisoning:
- Performing evaluation and/or intervention based on the blood lead levels:
- Below 20 mcg/dL:
- For asymptomatic children: provide long-term neurodevelopmental follow-up and counselling, while conduct periodic blood sampling to stabilize lead level until lower than 5 mcg/dL
- For symptomatic patients: measure blood lead level and review the child’s clinical status at least every 3 months, while treat iron deficiency promptly, and refer for environmental investigation and management
- Between 20 and 45 mcg/dL: lower the exposure to all sources of lead, correct any iron deficiency, maintain an adequate calcium intake, and frequently monitor to ensure the child’s blood lead levels are decreasing
- At or above 45 mcg/dL: Conduct chelation therapy after repeated blood lead measurement for confirmation, or immediately if encephalopathy is suspected
Monitoring the neurodevelopmental outcomes:
- Provide nutritional support, e.g. sufficient intake of calcium, vitamins C and D to minimize lead absorption
- Conduct preventive measures and education on lead exposure
- Follow up continuously with children at least after the environmental sources of lead have been identified and eliminated, with blood lead level declined to below 15 mcg/dL for not less than 6 months
- Monitor long-term neurodevelopment even a case is closed, until the child reached 6 years old
Link to full article: http://www.hkmj.org/abstracts/v23n6/616.htm
Reference
Hon KL, Fung CK, Leung AK. Childhood lead poisoning: an overview. Hong Kong Med J. 2017;23(6):616-21.
WYE-EM-010-JAN-18
If you liked this post you may also like